Understanding Health Risks
Improve Your Chances for Good Health
Risks are all around us. A nearby sneeze may raise your risk for catching the flu. Obesity boosts the odds you’ll get diabetes. Smoking increases your risk for many cancers. And if you pay attention to news headlines, you may worry that you’re at risk for food poisoning, Zika infection, shark attacks, and more. How can you know which health risks apply to you?
Health risks can sometimes be confusing, but they’re important to understand. Knowing the risks you and your family may face can help you find ways to avoid health problems. It can also keep you from fretting over unlikely threats. Knowing the risks and benefits of a medical treatment can help you and your doctor make informed decisions.
“Understanding health risks is key to making your own health care decisions,” says Dr. William Elwood, a psychologist and behavioral scientist at NIH. “It gives you perspective on potential harms and benefits, so you can make smart choices based on facts and not fears.”
A health risk is the chance or likelihood that something will harm or otherwise affect your health. Risk doesn’t mean that something bad will definitely happen. It’s just a possibility. Several characteristics, called risk factors, affect whether your health risks are high or low.
Your personal health risk factors include your age, sex, family health history, lifestyle, and more. Some risks factors can’t be changed, such as your A substance inherited from your parents that defines features such as your risk for certain diseases. genes or ethnicity. Others are within your control, like your diet, physical activity, and whether you wear a seatbelt.
When you see health statistics, consider the types of people being described. If they’re not similar to you, or if the category is very broad, then your risks may be different. A general statement like “More than half of Americans over age 45 will develop heart disease at some point” is based on statistical averages across the entire U.S. population. If you’re younger than 45, your heart disease risk will generally be much lower. The more risk factors you have—such as smoking, high blood pressure, or diabetes—the greater your risk. Exercise and a healthy diet, on the other hand, can make your chance of developing heart disease lower than for most other people.
“In many ways, our perception of risk is irrational,” says Elwood. “We sometimes worry over something that’s extremely unlikely, like Ebola in the U.S. And we ignore steps we can take to prevent what’s much more likely to harm us, like heart disease or colon cancer.”
Talking about health risks can seem intimidating. Even doctors sometimes have trouble with risk concepts. That’s why NIH supports research to improve how medical staff and others communicate health risks and prevention strategies to patients and the public.
“Math in general is hard for a lot of people. Yet math is often hidden in everyday activities that affect our health,” says Dr. Russell Rothman, a physician and scientist at Vanderbilt University in Nashville. Rothman’s research focuses on helping people understand and work with numbers, so they can reduce their risks for diabetes and excess weight, including childhood obesity.
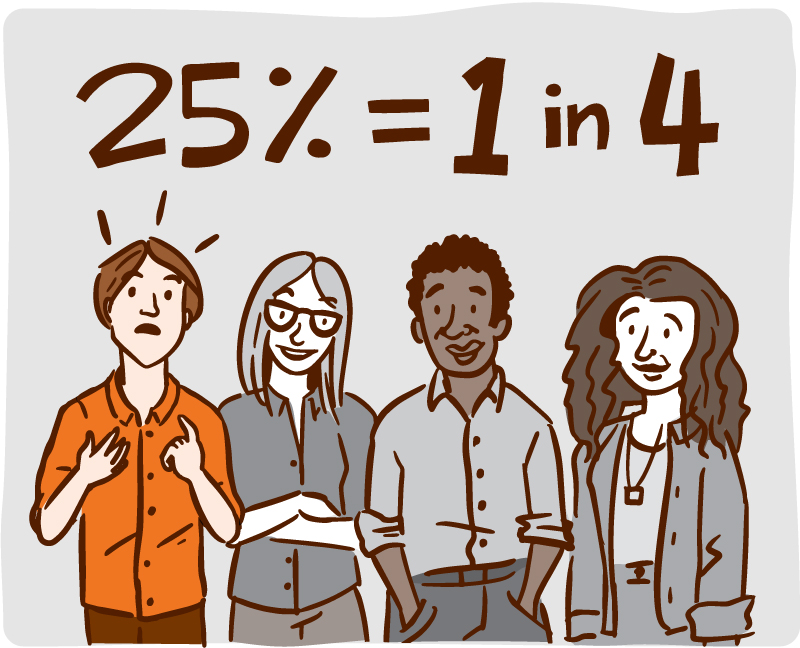
Studies show that the way we hear and understand health statistics can be influenced by how the numbers are described, or how they’re “framed.” Different descriptions can affect how clear the information is and also what emotions it stirs. For example, the statement: “More than 20% of Americans will eventually die of cancer” might sound less scary from a different perspective: “Nearly 80% of Americans will not die of cancer.” The same information might seem clearer described as a ratio: “More than 1 in 5 Americans will eventually die of cancer.” Research shows that pictures or diagrams are often the most understandable—for instance, showing 5 human figures with 1 in a different color.
To understand the potential risks or benefits of a medical treatment or behavior change, it helps to focus on a math concept called “absolute risk.” Absolute risk is the chance of something happening, such as a health problem that might arise over a period of time. For example, a disease might affect 2 in 100 middle-aged men over their lifetimes. If a certain drug lowers their risk for the disease to 1 in 100, the drug has reduced their absolute risk by 1 person in 100, or 1%. Another way to think of it is that you’d need to treat 100 people with this medicine to prevent just 1 additional person from getting the disease.
Often, however, you might hear numbers that use a related concept called “relative risk.” Relative risk compares the absolute risks of one group to another. In the example above, you could also say that the drug reduced the risk of disease by 50%, since 1 is half of 2. Looking at relative risk alone, you may mistakenly think that the drug is highly effective.
“Many times, the relative risk sounds much greater than the absolute risk, which can be confusing,” Rothman explains. When you hear numbers about risk, it’s best to focus on the absolute risk.
Health risks can be especially hard to grasp when emotions run high, such as when people are faced with a serious illness. One recent NIH-funded study found that people with advanced cancer tended to expect better outcomes and longer survival times from treatment than their doctors did. Most patients didn’t realize that their outlook differed from their doctors. Such misunderstandings might affect whether patients choose to undergo harsh treatments.
“Communication is a 2-way street,” says the study’s lead researcher, Dr. Ronald M. Epstein of the University of Rochester Medical Center in New York. “For effective discussions to occur, doctors must provide encouragement and answers. And patients have to ask important questions.” Epstein and colleagues are developing methods to help doctors and patients have realistic discussions about topics such as emotions, treatment choices, and likely outcomes.
“We’ve shown it’s possible to improve the conversations. It helps if patients come prepared with 3 or 4 big-picture questions to ask their doctors,” Epstein says. For people with advanced cancer, questions might include: How will treatment affect my quality of life? What’s the average survival time for this type of cancer?
“It can feel scary to ask those kinds of questions. Sometimes you don’t really want to know the answers, or you have mixed feelings,” Epstein says. “Doctors can help by opening the door to conversation. They can say, ‘Tell me what’s on your mind. Do you have any questions?’” Such open conversations can help patients and their families make more informed health decisions.
Start by talking with your doctor about your health risks. Ask how you can reduce your risks. And look to trustworthy websites—like NIH’s health.nih.gov—for reliable health information.
NIH Office of Communications and Public Liaison
Health and Science Publications Branch
Building 31, Room 5B52
Bethesda, MD 20892-2094
Contact Us:
nihnewsinhealth@od.nih.gov
Phone: 301-451-8224
Share Our Materials: Reprint our articles and illustrations in your own publication. Our material is not copyrighted. Please acknowledge NIH News in Health as the source and send us a copy.
For more consumer health news and information, visit health.nih.gov.
For wellness toolkits, visit www.nih.gov/wellnesstoolkits.




