The Power of Your Pancreas
Keep Your Digestive Juices Flowing
How much you eat alters more than your waistline. It also affects your body’s organs, starting with your pancreas. With each bite, your pancreas must release enough digestive juices and hormones for you to benefit from the food you eat. Putting too much stress on your pancreas—by too much eating, drinking, or smoking—can cause serious health issues.
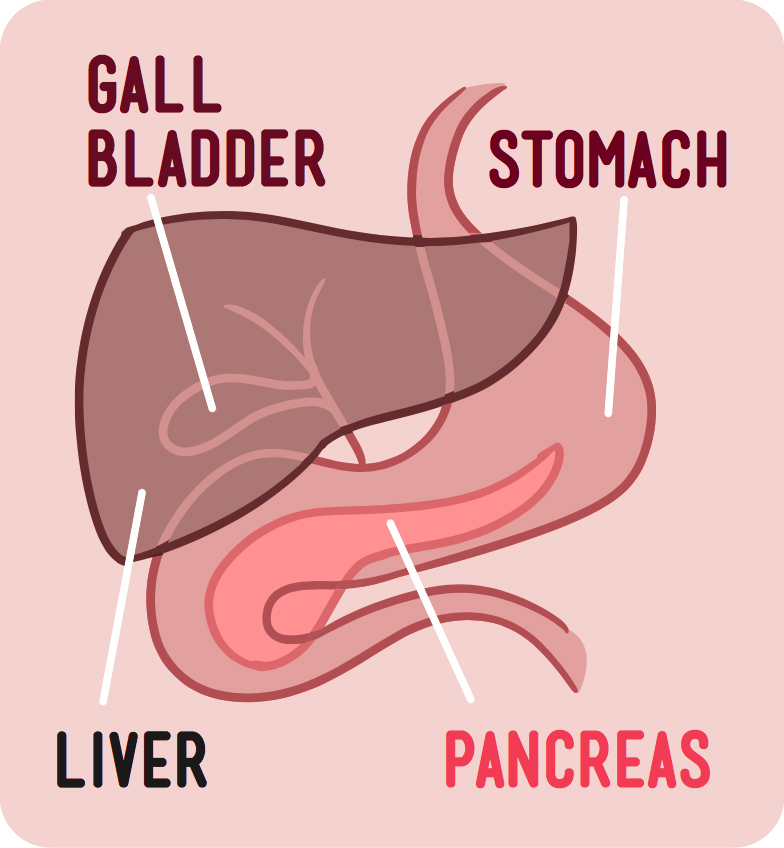
The pancreas lies behind your stomach. It’s surrounded by the intestines, liver, and gallbladder. These neighboring organs work together to help you digest your food.
“The pancreas produces a variety of enzymes to help break down the carbohydrates, proteins, and fats in your diet into smaller elements that are more easily used for energy,” says Dr. Dana Andersen, a pancreatic specialist at NIH. “It also produces specialized hormones that travel through the blood and help regulate a variety of body functions.”
The best known hormone produced by the pancreas is insulin. Insulin controls how much sugar, or glucose, is taken up by your body’s cells. If the insulin-producing cells in the pancreas are damaged, diabetes may arise. Type 2 diabetes occurs when the pancreas can’t produce enough insulin to handle the sugar in your blood. Obesity worsens type 2 diabetes.
“Obesity can make your body less sensitive to insulin, so it takes more insulin to achieve the same metabolic work. That puts more stress on the pancreas,” Andersen says. “Just losing 5 or 10 pounds can help the pancreas to work more efficiently.”
High levels of fat in the blood can also lead to Swelling and irritation caused by the body’s protective response to injury. inflammation of the pancreas, or pancreatitis, which can be chronic or acute. With chronic pancreatitis, the inflammation doesn’t heal and gets worse over time. Eventually, it can lead to permanent damage.
Acute pancreatitis occurs suddenly and is very painful. It usually resolves in a few days with treatment. In severe cases, bleeding and permanent tissue damage may occur. The most common causes of acute pancreatitis are gallstones and heavy alcohol use. Gallstones are small, pebble-like substances made of hardened bile (a liquid produced by the liver to digest fat). Other causes of acute pancreatitis include abdominal trauma, medications, and infections.
Genetic disorders of the pancreas and certain Condition in which the body’s immune system mistakenly attacks the body’s own cells and tissues. autoimmune disorders can also lead to pancreatitis. But in nearly half of cases, the cause is unknown—a condition known as idiopathic pancreatitis.
Tracking your family’s medical history can help you learn if you’re at risk for pancreatic problems. “It’s always a good idea to tell your doctor if there’s been a family history of pancreatic disease,” Andersen says. “That may not sound like much, but to a doctor it’s very important information.”
Knowledge of family health history is especially important for possible early detection of pancreatic cancer, which usually has no symptoms in its early stages. When caught early, pancreatic cancer may be curable with surgery. But most patients with pancreatic cancer aren’t diagnosed until more advanced stages, when the chances for survival are low.
NIH researchers are looking for new ways to detect pancreatic diseases early and predict who’s most at risk. Eating a healthy diet and limiting your exposure to harmful substances, like tobacco and alcohol, can help keep your pancreas and your entire digestive system working properly.
NIH Office of Communications and Public Liaison
Health and Science Publications Branch
Building 31, Room 5B52
Bethesda, MD 20892-2094
Contact Us:
nihnewsinhealth@od.nih.gov
Phone: 301-451-8224
Share Our Materials: Reprint our articles and illustrations in your own publication. Our material is not copyrighted. Please acknowledge NIH News in Health as the source and send us a copy.
For more consumer health news and information, visit health.nih.gov.
For wellness toolkits, visit www.nih.gov/wellnesstoolkits.




